Male Infertility: Causes and Investigations

Male infertility is a health condition that impedes a man's ability to initiate a pregnancy with his female partner. This condition is often associated with complications in sperm production or the creation of healthy sperm. It can also be linked to functional issues that affect the sperm's capacity to fertilize an egg. The causes of male infertility are multifaceted and can include hormonal imbalances, genetic disorders like cystic fibrosis, problems with the testes, and blockages in the genital tract. Environmental factors, lifestyle choices such as smoking or excessive alcohol consumption, infections, certain medications, and sexual dysfunction can also contribute to male infertility. A comprehensive medical evaluation by a specialist, such as a urologist or reproductive endocrinologist, is typically required for accurate diagnosis and effective treatment of this condition.
Male Reproductive System
The male reproductive system is a complex network of organs and structures that work in harmony to ensure the production, maturation, and delivery of spermatozoa.
- Testes: These paired organs, nestled within the scrotal sac, serve as the epicenter of male reproductive function. Their dual role involves both sperm production (spermatogenesis) and the secretion of testosterone—the quintessential male hormone. The testes are home to specialized cells called Leydig cells, which diligently manufacture testosterone.
- Ductal System:
- Epididymis: A coiled tube adjacent to each testis, the epididymis plays a pivotal role in sperm maturation. It provides a nurturing environment for spermatozoa, allowing them to gain motility and acquire the ability to fertilize an egg.
- Vasa Deferentia: These paired ducts extend from the epididymis and serve as conduits for sperm transport. They propel sperm toward their ultimate destination—the ejaculatory ducts.
- Ejaculatory Ducts: These tubes, formed by the union of the vasa deferentia and seminal vesicles, facilitate the release of sperm during ejaculation. Their intricate coordination ensures the efficient delivery of spermatozoa.
- Accessory Glands:
- Seminal Vesicles: Paired and strategically positioned near the base of the bladder, the seminal vesicles contribute significantly to seminal fluid composition. Their secretions provide nourishment and energy to sperm, enhancing their chances of survival.
- Prostate Gland: Singular and walnut-sized, the prostate gland adds its own unique blend to the seminal fluid. Its contributions include enzymes and substances that aid in liquefying semen post-ejaculation.
- Bulbourethral Glands of Cowper: These small glands, often overlooked, secrete a lubricating mucus. This mucus serves as a prelude to ejaculation, ensuring smooth passage for sperm through the urethra.
- Penis: The external organ of copulation, the penis plays a dual role: it houses the urethra (through which urine and semen exit) and serves as the conduit for sexual intercourse.
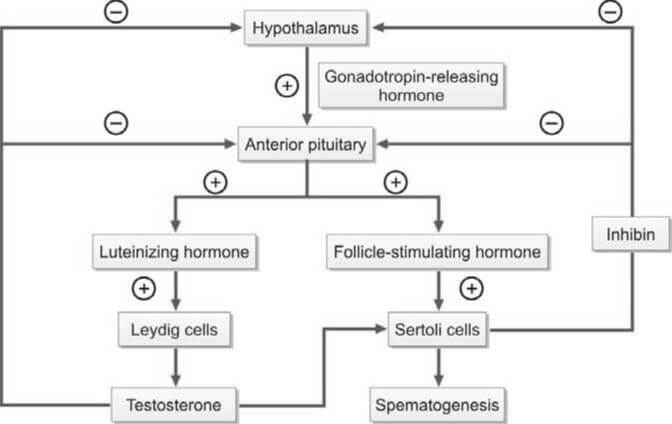
- Hormonal Regulation:
- Gonadotropin-Releasing Hormone (GnRH): Produced by the hypothalamus, GnRH orchestrates the delicate dance of hormonal regulation. It stimulates the anterior pituitary gland to release two crucial gonadotropins: luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- Luteinizing Hormone (LH): LH's primary target is the Leydig cells within the testes. Upon activation, these cells ramp up testosterone production, essential for spermatogenesis and the development of secondary sexual characteristics.
- Testosterone: This powerhouse hormone not only fuels sperm production but also influences muscle mass, bone density, and libido. Intriguingly, testosterone undergoes conversion to dihydrotestosterone (DHT) within cells, enabling it to exert its androgenic effects.
- Follicle-Stimulating Hormone (FSH): Acting on Sertoli cells within the seminiferous tubules, FSH fine-tunes the maturation process of spermatozoa. These same Sertoli cells also produce inhibin, which, in a neat feedback loop, regulates FSH secretion.
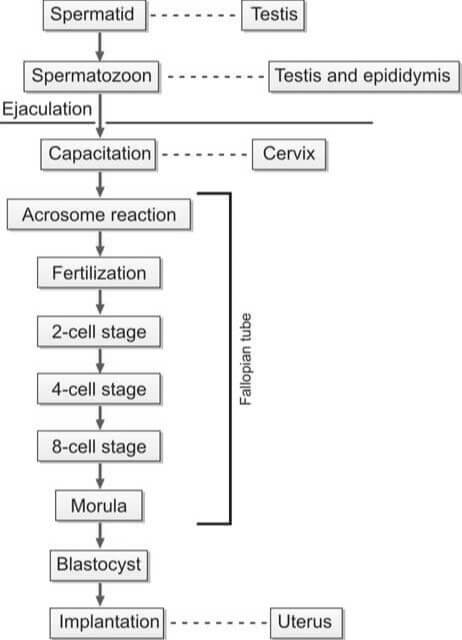
During the act of copulation, seminal fluid is introduced into the female's vagina. This semen undergoes a process known as liquefaction within a span of 20 to 30 minutes, facilitated by the proteolytic enzymes present in the prostatic fluid. For successful in vivo fertilization, the spermatozoa must experience capacitation and the acrosome reaction.
Capacitation is a term that describes the physiological transformations that sperm undergo as they traverse the cervix of the female reproductive tract. Through this process, the sperm gain the ability to (i) initiate the acrosome reaction, (ii) bind to the zona pellucida, and (iii) exhibit hypermotility. The sperm then journey through the cervix and uterus, eventually reaching the fallopian tube.
The binding of the sperm to the zona pellucida triggers the acrosomal reaction, which involves the breakdown of the outer plasma membrane by acrosomal enzymes and its fusion with the outer acrosomal membrane, resulting in the loss of the acrosome. This step is crucial for the fusion of the sperm and oocyte membranes.
Following the acrosomal reaction and the binding of sperm and ovum surface proteins, the sperm penetrates the zona pellucida of the ovum. After a sperm has penetrated, the zona pellucida hardens, preventing further penetration by additional sperm. The fertilization of the egg by the sperm typically occurs in the ampullary section of the fallopian tube.
Factors Contributing to Male Infertility
Male infertility is a complex issue that arises from a multitude of factors that can impact sperm production, motility, or function. It’s often rooted in hormonal imbalances, genetic disorders such as Klinefelter syndrome, and testicular complications including trauma or cancer. Environmental influences, including exposure to harmful toxins, can also play a part. Lifestyle choices, such as smoking, excessive alcohol consumption, and obesity, significantly contribute to male infertility. Furthermore, infections, certain medications, and sexual dysfunction can also be contributing factors. To accurately identify the specific cause, a comprehensive medical evaluation by a urologist or reproductive specialist is typically necessary. Understanding the root cause is the first step towards effective treatment and management of male infertility.
The following are the various factors that can contribute to male infertility:
- Idiopathic: This refers to cases where the cause of infertility remains unknown.
- Hypothalamic-Pituitary Dysfunction (Hypogonadotropic Hypogonadism): This condition involves a disruption in the communication between the hypothalamus and pituitary gland, leading to decreased production of sex hormones.
- Testicular Dysfunction: This category includes a variety of factors:
- Exposure to radiation, cytotoxic drugs, antihypertensives, and antidepressants.
- General factors such as stress, emotional factors, substance abuse (including marijuana, anabolic steroids, and cocaine), alcoholism, heavy smoking, and undernutrition.
- Post-puberty mumps orchitis.
- Varicocele, which is the dilation of the pampiniform plexus of scrotal veins.
- Cryptorchidism, or undescended testes.
- Endocrine disorders such as diabetes mellitus and thyroid dysfunction.
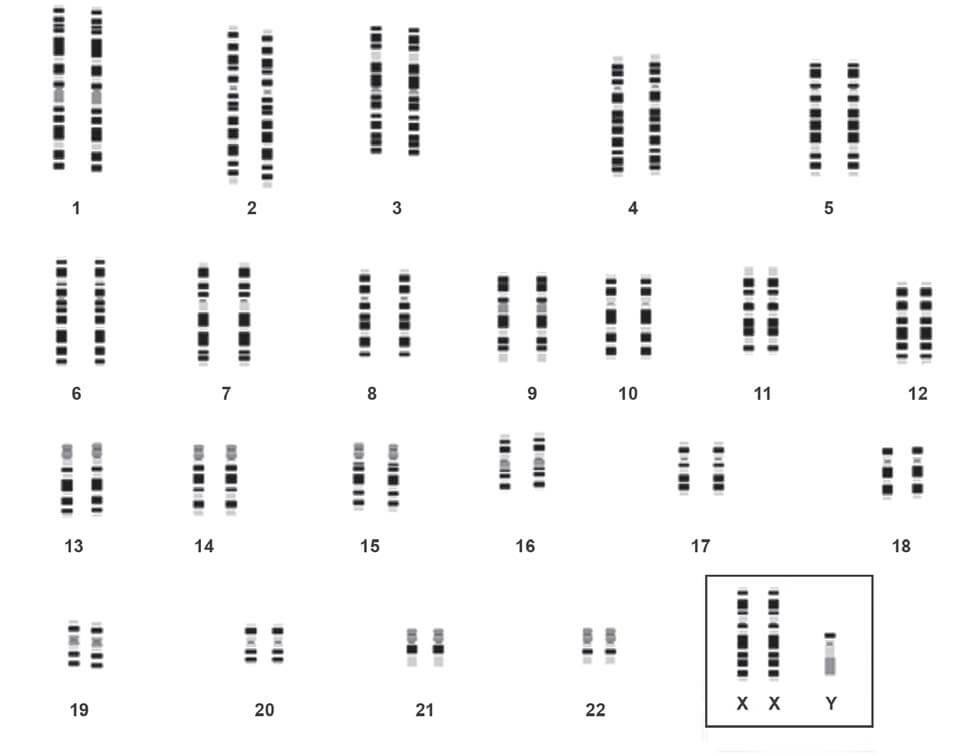
- Genetic disorders including Klinefelter’s syndrome, microdeletions in the Y chromosome, autosomal Robertsonian translocation, immotile cilia syndrome (Kartagener’s syndrome), cystic fibrosis, and defects in the androgen receptor gene.
- Dysfunction of Passages and Accessory Sex Glands: This includes:
- Infections of the epididymis caused by tuberculosis, gonorrhea, or Chlamydia.
- Congenital bilateral absence of the vasa deferentia (often associated with cystic fibrosis) or vasectomy.
- Prostatitis, or inflammation of the prostate gland.
- Dysfunction of Sexual Act: This encompasses:
- Impotence or erectile dysfunction.
- Ejaculation defects such as retrograde ejaculation (where semen is pumped backwards into the bladder), premature ejaculation, or absence of ejaculation.
- Hypospadias, a condition where the opening of the urethra is on the underside of the penis rather than at the tip.
Examination Procedures for Male Infertility
The following are the various procedures involved in the investigation of male infertility:
- Patient History: This encompasses the individual's lifestyle (including heavy smoking and alcohol consumption), sexual habits, instances of erectile dysfunction, ejaculation patterns, history of sexually transmitted diseases, any surgeries performed in the genital area, medication usage, and any systemic illnesses.
- Physical Examination: This involves a thorough examination of the reproductive system, including the size of the testicles, presence of undescended testes, hypospadias, and any scrotal abnormalities such as varicocele. It also includes an assessment of body and facial hair. Varicocele, which can occur bilaterally, is the most common surgically correctable abnormality causing male infertility.
- Semen Analysis: Please refer to the article on Semen Analysis for more information. The evaluation of azoospermia and low semen volume are depicted in Flowcharts 3 and 4, respectively.
- Chromosomal Analysis: This test can identify conditions such as Klinefelter’s syndrome (e.g., XXY karyotype), deletions in the Y chromosome, and autosomal Robertsonian translocations. If there is a bilateral congenital absence of the vas deferens, screening for the cystic fibrosis carrier state is necessary.
- Hormonal Studies: These involve the measurement of FSH, LH, and testosterone levels to detect any hormonal abnormalities that could lead to testicular failure.
- Testicular Biopsy: A testicular biopsy is recommended when it is not clear whether azoospermia is obstructive or non-obstructive (i.e., normal FSH levels and normal testicular volume).
| Follicle stimulating hormone | Luteinizing hormone | Testosterone | Interpretation |
|---|---|---|---|
| Low | Low | Low | Hypogonadotropic hypogonadism (Hypothalamic or pituitary disorder) |
| High | High | Low | Hypergonadotropic hypogonadism (Testicular disorder) |
| Normal | Normal | Normal | Obstruction of passages, dysfunction of accessory glands |
- Azoospermia (on two separate occasions)
- Normal-sized testes
- Obstructive azoospermia
- Epididymal obstruction by chlamydia or gonorrhea
- Vasectomy
- Congenital bilateral absence of vas
- Genetic testing for cyctic fibrosis gene
- Obstructive azoospermia
- Small or soft testes
- Non-obstructive azoospermia
- Hormonal analysis
- FSH, LH, testosterone levels low
- Hypogonadotropic hypogonadism
- FSH, LH high; testosterone level normal or low
- Primary testicular failure
- Genetic studies for Klinefelter's syndrome
- Primary testicular failure
- FSH, LH, testosterone levels low
- Hormonal analysis
- Non-obstructive azoospermia
- Normal-sized testes
- Semen volume <1ml
- Examination of post-ejaculatory urine
- Positive for sperms
- Retrograde ejaculation
- Negative for sperms
- Transrectal ultrasonography for seminal vesicle abnormality and ejaculatory duct obstruction
- Positive for sperms
- Examination of post-ejaculatory urine
The following are the standard preliminary examinations typically conducted to determine the cause of infertility:
- Semen Analysis: This is a comprehensive examination of a man's semen and sperm to assess fertility.
- Blood Glucose: This test measures the level of glucose (sugar) in the blood and can indicate potential health issues.
- Endocrine Tests: These tests measure the levels of specific hormones in the blood, such as Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH), and testosterone, which play crucial roles in reproduction.
References
- Brugh III, VM, Lipshultz LI. Male factor infertility: Evaluation and management. Med Clin N Am 2004;88:367-85.
- Burtis CA, Ashwood ER. Tietz fundamentals of clinical chemistry. 5th Ed. Philadelphia: WB Saunders Company, 2001.
- Dohle GR, Jungwirth A, Colpi G, Papp G, Pomerol J, Hargreave TB. Guidelines on male infertility. European Association of Urology, 2006.
- Hamilton-Fairley D, Taylor A. Anovulation. BMJ 2003;327:546-9.
- Jarrow JP. Diagnostic approach to the infertile male patient. Endocrinol Metab Clin N Am 2007;36:297-311.
- Khalaf Y. Tubal subfertility. BMJ 2003;327:610-3.
- Kolettis PN. Evaluation of the subfertile man. Am Fam Physician 2003;67:2165-73.
- Williams C, Giannopoulos T, Sherriff EA. Investigation of infertility with the emphasis on laboratory testing and with reference to radiological imaging. J Clin Pathol 2003;56:261-7.
- Comment
- Posted by Dayyal Dg.